Connect With Us
Blog

How the Arches of the Foot Work
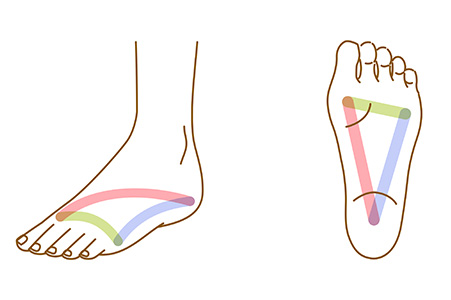
The arches of the foot play a significant role in movement, stability, and shock absorption. The foot has three arches, the medial longitudinal arch, the lateral longitudinal arch, and the transverse arch. These structures are formed by the tarsal and metatarsal bones and are supported by ligaments and tendons. The medial arch, which is the highest and most flexible, distributes weight and adapts to changes in terrain. The lateral arch is lower and provides stability, while the transverse arch helps maintain foot shape and balance. A well-functioning arch system allows efficient weight distribution and reduces strain on the joints. However, arch abnormalities can lead to pain and dysfunction. A low arch, or flat foot, often results in excessive foot pronation, which increases the risk of heel pain and arch discomfort. A high arch may reduce shock absorption, placing excessive pressure on the forefoot and heel. A podiatrist can evaluate your foot’s arch structure, diagnose potential issues, and provide treatment options like custom orthotics, or, in severe cases, surgery. If you are experiencing pain in the arch of your foot, it is suggested that you schedule an appointment with a podiatrist for an exam, diagnosis, and treatment options.
If you have any concerns about your feet, contact one of our podiatrists from Kokomo Foot & Ankle Center. Our doctors can provide the care you need to keep you pain-free and on your feet.
Biomechanics in Podiatry
Podiatric biomechanics is a particular sector of specialty podiatry with licensed practitioners who are trained to diagnose and treat conditions affecting the foot, ankle and lower leg. Biomechanics deals with the forces that act against the body, causing an interference with the biological structures. It focuses on the movement of the ankle, the foot and the forces that interact with them.
A History of Biomechanics
- Biomechanics dates back to the BC era in Egypt where evidence of professional foot care has been recorded.
- In 1974, biomechanics gained a higher profile from the studies of Merton Root, who claimed that by changing or controlling the forces between the ankle and the foot, corrections or conditions could be implemented to gain strength and coordination in the area.
Modern technological improvements are based on past theories and therapeutic processes that provide a better understanding of podiatric concepts for biomechanics. Computers can provide accurate information about the forces and patterns of the feet and lower legs.
Understanding biomechanics of the feet can help improve and eliminate pain, stopping further stress to the foot.
If you have any questions please feel free to contact our office located in Contact Us . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Biomechanics in Podiatry
Podiatry is a branch of medicine that deals with the study, diagnosis, and treatment of foot and ankle conditions. There are various subdivisions in podiatry; biomechanics is one of them. Biomechanics is the way in which the bones, muscles, and joints of the feet and lower limb interact with each other.
Our feet play crucial roles in the way we move, and it is rare to have feet that are completely symmetrical. Common biomechanical issues include high or low arches or uneven leg heights. Excessive pronation often leads to fallen arches, or flat feet, and is a common cause of running injuries. People whose feet are over-pronated tend to have flexible and unstable feet. Pain is usually experienced during walking and running.
At times, people may be able to adapt to these abnormalities without any difficulties, but in other cases, these issues can cause a great deal of pain. This pain occurs because the joints, muscles, ligaments, and tendons are put under an excess amount of stress during movement. Common symptoms of biomechanical problems stemming from the feet include hip pain, knee pain, leg cramps, ankle pain, lower back pain, weak ankles, tripping, heel pain, Achilles pain, and shin splints.
Many biomechanical issues can be treated with orthotics. Orthotics are shoe insoles that are used to help control the way the foot operates. They can provide relief from foot pain, heel pain, and knee pain. Depending on your specific case, you may need to purchase over-the-counter orthotics or custom orthotics to fit your feet. Your podiatrist will be able to prescribe the perfect orthotic for your feet to help you walk around with ease.
Gait is defined as the way we move our bodies from one point to another. This is usually done by either walking or running. Gait analysis is a method used to assess the way we walk or run to highlight biomechanical abnormalities. Gait analyses are a great way to take a detailed look at how you walk and how your foot moves while you walk. An examination of the feet will help your podiatrist understand why you are suffering pain in other parts of your body.
See Your Foot Specialist Regularly If You Work On Your Feet
The Hidden Dangers of Falls

Falls can lead to serious foot and ankle injuries, from sprains and fractures to long-term mobility issues. While anyone can fall, children and seniors are especially vulnerable. Kids, with their endless energy and unsteady coordination, often take tumbles, while aging adults face balance challenges and weaker bones. Surprisingly, men are more likely to die from a fall, while women are more likely to suffer lasting disabilities. Prevention is key. Seniors should focus on balance exercises, wearing proper footwear, and removing trip hazards at home. Good lighting, handrails, and assistive devices can also help. Children benefit from safe play areas, wearing non-slip socks, and learning to navigate stairs carefully. When falls do happen, injuries may not always seem severe at first. Ignoring them can lead to long-term damage. If foot or ankle pain lingers after a fall, it is suggested that you schedule an appointment with a podiatrist for evaluation and appropriate treatment.
Preventing falls among the elderly is very important. If you are older and have fallen or fear that you are prone to falling, consult with one of our podiatrists from Kokomo Foot & Ankle Center. Our doctors will assess your condition and provide you with quality advice and care.
Every 11 seconds, an elderly American is being treated in an emergency room for a fall related injury. Falls are the leading cause of head and hip injuries for those 65 and older. Due to decreases in strength, balance, senses, and lack of awareness, elderly persons are very susceptible to falling. Thankfully, there are a number of things older persons can do to prevent falls.
How to Prevent Falls
Some effective methods that older persons can do to prevent falls include:
- Enrolling in strength and balance exercise program to increase balance and strength
- Periodically having your sight and hearing checked
- Discuss any medications you have with a doctor to see if it increases the risk of falling
- Clearing the house of falling hazards and installing devices like grab bars and railings
- Utilizing a walker or cane
- Wearing shoes that provide good support and cushioning
- Talking to family members about falling and increasing awareness
Falling can be a traumatic and embarrassing experience for elderly persons; this can make them less willing to leave the house, and less willing to talk to someone about their fears of falling. Doing such things, however, will increase the likelihood of tripping or losing one’s balance. Knowing the causes of falling and how to prevent them is the best way to mitigate the risk of serious injury.
If you have any questions, please feel free to contact our office located in Contact Us . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Falls Prevention
Elderly Americans are very susceptible to falls as they get older. Everyone experiences decreases in flexibility, balance, strength, and the senses as they age. This correlates to some eye-opening statistics. 1 in 4 Americans aged 65 and older fall each year. An elderly American is being treated for a fall in an emergency room every 11 seconds. In light of these striking statistics, one can see the importance of taking steps to prevent falls.
Finding an exercise program for the elderly is an excellent way to reduce the likelihood of falls. Look for an exercise program that improves strength and balance. Elderly people who live a more sedentary lifestyle, with little physical activity, are at an increased risk of falling. Wearing well-fitted footwear that provides good foot support and cushion will help prevent falls from poorly fitted shoes. Talking to a podiatrist about your susceptibility to falls and about inspecting your prescriptions will help to avoid any medication that could make falls more likely. Due to a decline in the senses among the elderly, having your eyes and hearing checked is recommended.
Around half of all falls occur in the household. Removing tripping hazards in the home and making it more accommodating to older persons can significantly reduce falls. Some notable household changes include increasing lighting around the house, installing grab bars in the shower and bathroom, and making sure the floor is clear of clutter. Other smart options include installing a shower chair, using rubber-bottomed rugs, and placing railings on both sides of stairwells.
Finally, discuss with a doctor and your family about your fear of falling. This will help to increase awareness among the population on the need for fall prevention. A lack of awareness on the matter, and a downplaying of importance are what increase the risks of falling. Following these tips can help to reduce the risk for yourself and your loved ones.
What Is a Blood Blister?

Blood blisters and regular blisters both form in response to friction, but they differ in appearance and severity. A regular blister is filled with clear fluid and typically forms when skin rubs against something repeatedly, causing the outer layer of skin to separate. Blood blisters, on the other hand, occur when a blood vessel beneath the skin breaks, causing the blister to fill with blood rather than fluid. This can also indicate that the blister is infected. Blood blisters can feel more painful, as they put pressure on the surrounding tissue. Both types of blisters can cause discomfort, swelling, and redness. It is important to keep both clean and covered to avoid further friction. Do not pop the blister as that can increase the risk of further infection. If a blood blister does not heal, a podiatrist can safely drain it, provide wound care, and advise on prevention strategies. For persistent or painful blisters, it is suggested that you schedule an appointment with a podiatrist to ensure proper care.
Blisters are prone to making everyday activities extremely uncomfortable. If your feet are hurting, contact one of our podiatrists of Kokomo Foot & Ankle Center. Our doctors can provide the care you need to keep you pain-free and on your feet.
Foot Blisters
Foot blisters develop as a result of constantly wearing tight or ill-fitting footwear. This happens due to the constant rubbing from the shoe, which can often lead to pain.
What Are Foot Blisters?
A foot blister is a small fluid-filled pocket that forms on the upper-most layer of the skin. Blisters are filled with clear fluid and can lead to blood drainage or pus if the area becomes infected.
How Do Blisters Form?
Blisters on the feet are often the result of constant friction of skin and material, usually by shoe rubbing. Walking in sandals, boots, or shoes that don’t fit properly for long periods of time can result in a blister. Having consistent foot moisture and humidity can easily lead to blister formation.
Prevention & Treatment
It is important to properly care for the affected area in order to prevent infection and ease the pain. Do not lance the blister and use a Band-Aid to provide pain relief. Also, be sure to keep your feet dry and wear proper fitting shoes. If you see blood or pus in a blister, seek assistance from a podiatrist.
If you have any questions, please feel free to contact our office located in Contact Us . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Blisters
Blisters are pockets of fluid that occur under the top layer of your skin. These fluid pockets are usually filled with pus, blood, or serum. Blisters may itch or hurt and can appear as a single bubble or in clusters.
The most common types of blisters are friction blisters. This type of blister may be caused by wearing shoes that are too tight. Friction blisters can also occur on the hands. A change in temperature may also cause blisters on the feet. In the freezing air, frostbite on your toes can lead to blisters, as well as sunburn from hot weather.
The best way to treat a blister is to keep it clean and dry. Most blisters will get better on their own. Once the skin absorbs the fluid within the blister, it will flatten and eventually peel off. You should avoid popping your blister unless you podiatrist does it for you. Additional treatment options include applying an ice pack to the blister or using over-the-counter blister bandages to cover the affected area.
If your blister becomes discolored, inflamed, or worsens it is advised that you speak to your podiatrist. Blisters that are yellow, green, or purple may be infected and require immediate medical attention. Blisters that are abnormally colored may be a sign of a more serious underlying health condition such as herpes.
Surgery for Tarsal Tunnel Syndrome

Tarsal tunnel syndrome happens when the tibial nerve is compressed inside the tarsal tunnel, a narrow space in the ankle. It causes tingling, burning, numbness, or sharp pain in the foot, often worsening with activity. People with flat feet, diabetes, arthritis, or previous ankle injuries are more likely to develop it. Doctors diagnose tarsal tunnel syndrome with a physical exam, nerve conduction tests, and sometimes imaging like an MRI scan. When conservative treatments like rest, orthotics, and targeted exercises do not help, surgery may be an option. Tarsal tunnel release surgery involves cutting the ligament over the nerve to relieve pressure. This can reduce pain and prevent further nerve damage. Recovery and satisfaction with the surgery varies, but exercises may help restore strength and movement. If you have persistent foot pain or numbness, it is suggested that you see a podiatrist for a proper diagnosis and treatment.
Tarsal tunnel syndrome can be very uncomfortable to live with. If you are experiencing tarsal tunnel syndrome, contact one of our podiatrists of Kokomo Foot & Ankle Center. Our doctors can provide the care you need to keep you pain-free and on your feet.
Tarsal Tunnel Syndrome
Tarsal tunnel syndrome, which can also be called tibial nerve dysfunction, is an uncommon condition of misfiring peripheral nerves in the foot. The tibial nerve is the peripheral nerve in the leg responsible for sensation and movement of the foot and calf muscles. In tarsal tunnel syndrome, the tibial nerve is damaged, causing problems with movement and feeling in the foot of the affected leg.
Common Cause of Tarsal Tunnel Syndrome
- Involves pressure or an injury, direct pressure on the tibial nerve for an extended period of time, sometimes caused by other body structures close by or near the knee.
- Diseases that damage nerves, including diabetes, may cause tarsal tunnel syndrome.
- At times, tarsal tunnel syndrome can appear without an obvious cause in some cases.
The Effects of Tarsal Tunnel Syndrome
- Different sensations, an afflicted person may experience pain, tingling, burning or other unusual sensations in the foot of the affected leg.
- The foot muscles, toes and ankle become weaker, and curling your toes or flexing your foot can become difficult.
- If condition worsens, infections and ulcers may develop on the foot that is experiencing the syndrome.
A physical exam of the leg can help identify the presence of tarsal tunnel syndrome. Medical tests, such as a nerve biopsy, are also used to diagnose the condition. Patients may receive physical therapy and prescriptive medication. In extreme cases, some may require surgery.
If you have any questions please feel free to contact our office located in Contact Us . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Tarsal Tunnel Syndrome
Tarsal tunnel syndrome is a condition in which there is a compression of the posterior tibial nerve. The posterior tibial nerve runs along the inside of the ankle into the foot. Tarsal tunnel syndrome is named for the tarsal tunnel, which is a thin space along the inside of the ankle beside the ankle bones. This space contains various nerves, arteries, and tendons, and includes the posterior tibial nerve. The tibial nerve is the peripheral nerve in the leg responsible for sensation and movement of the foot and calf muscles. In tarsal tunnel syndrome the tibial nerve is compressed, causing tingling or burning, numbness, and pain.
Common causes of tarsal tunnel syndrome involve pressure or an injury. Injuries that produce inflammation and swelling in or around the tunnel may place pressure on the posterior tibial nerve. Direct pressure on the tibial nerve for an extended period of time, sometimes caused by other body structures close by or trauma to the tibial nerve, can result in tarsal tunnel syndrome. Diseases that damage nerves, such as diabetes or arthritis, may cause tarsal tunnel syndrome. Those with flat feet are at risk for developing the condition, as the extra pressure and strain placed on the foot may compress the posterior tibial nerve.
Feeling different sensations in the foot at different times is a common symptom of tarsal tunnel syndrome. An afflicted person may experience pain, tingling, burning or other unusual sensations in the foot of the affected leg. Symptoms are primarily felt on bottom of the foot and/or the inside of the ankle. Symptoms can appear suddenly and may occur due to overuse of the foot.
To diagnose tarsal tunnel syndrome, your podiatrist may examine the foot and tap the posterior tibial nerve to see if symptoms surface. He or she may also order an MRI to determine if a mass is present.
Treating tarsal tunnel syndrome will depend on the decision of your podiatrist. Multiple options are available, however, and can include rest, ice, immobilization, oral medications such as anti-inflammatory drugs (NSAIDS), physical therapy, injection therapy, orthotics, supportive shoes, braces, and surgery.
Explanation of Plantar Fasciitis

Plantar fasciitis is caused by inflammation of the plantar fascia, the thick band of tissue that runs along the bottom of your foot from the heel to the toes. It is often triggered by repetitive stress, wearing improper footwear, or excessive pressure on the feet. Symptoms include sharp heel pain, especially with the first few steps in the morning or after long periods of rest. The pain may improve as you move, but it often returns after prolonged standing or walking. Swelling and tenderness at the heel are also common. Treatment for plantar fasciitis typically involves rest, exercises, and mild pain relievers. A podiatrist may recommend custom orthotics or corticosteroid injections for persistent cases. In rare cases, surgery may be necessary. This type of doctor can help diagnose and guide you through effective treatments for plantar fasciitis. If you are experiencing this condition, it is suggested that you schedule an appointment with a podiatrist.
Plantar fasciitis is a common foot condition that is often caused by a strain injury. If you are experiencing heel pain or symptoms of plantar fasciitis, contact one of our podiatrists from Kokomo Foot & Ankle Center. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is one of the most common causes of heel pain. The plantar fascia is a ligament that connects your heel to the front of your foot. When this ligament becomes inflamed, plantar fasciitis is the result. If you have plantar fasciitis you will have a stabbing pain that usually occurs with your first steps in the morning. As the day progresses and you walk around more, this pain will start to disappear, but it will return after long periods of standing or sitting.
What Causes Plantar Fasciitis?
- Excessive running
- Having high arches in your feet
- Other foot issues such as flat feet
- Pregnancy (due to the sudden weight gain)
- Being on your feet very often
There are some risk factors that may make you more likely to develop plantar fasciitis compared to others. The condition most commonly affects adults between the ages of 40 and 60. It also tends to affect people who are obese because the extra pounds result in extra stress being placed on the plantar fascia.
Prevention
- Take good care of your feet – Wear shoes that have good arch support and heel cushioning.
- Maintain a healthy weight
- If you are a runner, alternate running with other sports that won’t cause heel pain
There are a variety of treatment options available for plantar fasciitis along with the pain that accompanies it. Additionally, physical therapy is a very important component in the treatment process. It is important that you meet with your podiatrist to determine which treatment option is best for you.
If you have any questions, please feel free to contact our office located in Contact Us . We offer the newest diagnostic and treatment technologies for all your foot care needs.